Malarial plasmodium in the human body - infection, symptoms and treatment
So, Plasmodium falciparum is the causative agent of malaria infection. According to the classification of protozoan (unicellular) parasites, it belongs to the phylum Apicomplexa, class Sporozoa, family Plasmodiidae, genus Plasmodium. And the English scientist Donald Ross discovered and experimentally proved the presence of a parasitic protozoan - malarial plasmodium in the saliva and intestines of a female mosquito of the genus Anopheles.
There are 4 types of parasites that can parasitize the human body:
- Plasmodium vivax is the causative agent of tertian malaria;
- Plasmodium malariae is the causative agent of four-day malaria;
- Plasmodium falciparum is the causative agent of tropical malaria;
- Plasmodium ovale is the causative agent of ovale malaria, similar to the species P. vivax.
All varieties are generally similar in shape, structure and life cycles. An interesting feature of parasites of the Apicomplexa type is the ability to alternate sexual (gamogony) and asexual (agamogony) methods of reproduction in the life cycle. In this case, a change of “master” occurs. In the human body, which is an “intermediate host” for the malarial plasmodium, only asexual reproduction is possible. And the phase of sexual reproduction is the prerogative of the main “host” and carrier of malaria, that is, the mosquito.
The female malaria mosquito is only a carrier of infection. When a person is bitten, the saliva of an infected mosquito enters the bloodstream, and sporozoites come with it. Symptoms of infection that manifest themselves in the disease are characteristic only of humans. Thus, the etiology of human malaria is infection when sporozoites of malarial plasmodium enter the blood.
Infection is possible in several ways:
- when bitten by a female Anopheles mosquito;
- during blood transfusion (hemotransfusion);
- for injections (through medical instruments);
- transplacental route (from a sick mother in labor to a child).
Periods and symptoms of the disease
The entire process, from infection to recovery, can be divided into four periods: incubation, acute, latent and relapse. The nature of the course of the disease and the frequency of relapses largely depend on the type of malarial plasmodium - the causative agent. For example, the incubation period of the disease can vary from 7 days to 1 year, depending on the type of malaria infection.
General characteristic signs of the disease:
- elevated body temperature (39 – 40 degrees); chills and fever replace each other;
- “ache” throughout the body;
- prolonged headaches;
- gagging and diarrhea;
- profuse sweating after a hot flash;
- severe enlargement of the liver and spleen;
- pain in the liver area;
- general weakness and anemia;
- possible confusion;
- yellowing of the skin and sclera of the eyes;
- frequent and painful urination;
- loss of appetite;
- insomnia.
Individual signs and symptoms (for example: cardiac stabbing pain, asthma attacks, joint pain) are also possible and depend on the presence of “weak points” in the body and the functioning of the immune system. Sick children usually develop a rash on their body. Tremors of the limbs are also typical for infants.
The initial symptoms of malaria can easily be mistaken for ARVI. But a very clear frequency of repetition of an attack of the disease (alternating chills and fever, ending with profuse sweating) is a distinctive feature of malaria and should be a signal to contact the clinic for advice. Especially if the patient has recently traveled and vacationed in countries with a hot tropical climate.
Diagnostics
In addition to the clinical assessment of the patient’s condition (based on the symptoms of the disease), laboratory methods for diagnosing malaria are used in medical practice. Malarial plasmodium manifests itself in blood tests at all stages of the disease before the onset of treatment. Therefore, special tests can determine its presence in the blood.
- The “thick drop of blood” method (Allows, at a minimum, to detect the presence of infection);
- Thin blood smear (Used to determine the type of malarial plasmodium - the pathogen and the stage of its development. This is necessary for the subsequent selection and prescription of drug treatment);
- Serological method (Detects the presence of antibodies to malaria in venous blood. A positive test result may also indicate a previous disease);
- PCR method - polymerase chain reaction (Used as an additional research method, along with the “thick drop” analysis, to detect malarial plasmodium at low concentrations in the blood).
In addition to specific diagnostic methods, the presence of infection is manifested in the form of deviations from the norm in a general blood test (hypochromic anemia, leukocytosis, thrombocytopenia). A general urine test also detects pathology based on indirect signs: hemoglobinuria and hematuria.
Traditional treatment
In medical practice, for the treatment of malaria, etiotropic therapy is used, aimed at localizing and combating the causative agent of the disease. For its effectiveness, preliminary laboratory diagnosis and correct selection of drugs are important. Depending on the type of malarial plasmodium and the stage of the disease, the patient may be prescribed various antimalarial drugs, as well as a combination of drugs.
Traditional medicine in the fight against malaria
Folk remedies for the treatment of malaria can be divided into basic and auxiliary, aimed at restoring the functioning of organs, detoxifying the body and increasing immunity.
Cinchona
The main and most effective means include treatment with cinchona bark powder. Here are two recipes for using this product:
- Take half a gram of quinine powder for five days exactly at sunrise. Then take a break for two days, and then resume taking the powder for another two days. An important condition is the need to sleep after taking the medicine.
- Prepare a fabric bag with quinine powder (10 grams of powder per bag) and place it on the patient’s chest for 3 to 4 hours. The medicine is absorbed by the body directly through the pores of the skin, which promotes rapid healing.
willow bark
Another effective treatment for malaria is the bark of willow branches. To prepare the medicine, you need to take a handful of bark and boil it in about three hundred ml of water until the volume of the liquid is reduced by one and a half times (to one glass). Take on an empty stomach for several days until the condition significantly improves. In addition to this recipe, it is also recommended to generously cover the patient’s bed with willow leaves during attacks, covering the top with a thin cloth.
Lilac and sunflower
Lilac leaves and sunflower inflorescences are also popular medicine remedies for malaria. An infusion of 20 lilac leaves in a glass of boiling water, kept warm for 1.5 hours, is taken twice a day, in the morning on an empty stomach and in the evening before bed, for 10 days.
Cut off the sunflower inflorescence when its petals begin to fall, chop it finely into a bottle and fill it with vodka. Cover the bottle with gauze, keep in a sunny place and leave for a month. Take 20 drops before the next attack or three times a day before meals.
Chicory and licorice
Good auxiliaries for quickly cleansing the lymphatic system and restoring the immune system are chicory root and licorice root.
Pour 10 grams of crushed licorice root into a container and add 200 ml of water. Keep in a water bath for half an hour. Cool the broth, strain and bring boiling water to 200 ml. You can drink the resulting decoction up to 5 times a day, at least an hour before meals. Portion for one serving – 5 tablespoons.
Preparation of chicory root decoction: pour 1 tablespoon of chicory root into 0.5 liters of water, bring to a boil and simmer for 20 minutes. Cool, strain and take 1 tablespoon three times a day before meals.
Garlic
Garlic is used as a natural antibiotic in the treatment of malaria. Preparation: Chop 2 peeled and washed heads of garlic and add a glass of cool, clean water. Leave for 12 hours. Take several sips during attacks while lying in bed. Approximately 1 glass per day for five days.
Prevention
Traditional medicine today cannot offer an effective vaccine against malaria. But research towards the development of such a vaccine is actively underway. To select a drug, it is important to know the type of pathogen that can be encountered in a given area, its resistance to the listed drugs, as well as possible side effects from taking the listed drugs. Any of the drugs must be taken at least a week before traveling to a disadvantaged region and continued for another month after leaving the danger zone.
Using mosquito nets, repellents (to repel mosquitoes), and mosquito killers reduces the risk of insect bites and infection.
At home, folk remedies are also used: peppermint, thyme, rosemary, geranium, basil, wormwood, lemon balm, cloves and eucalyptus. The smell of these plants repels dangerous insects.
Rapid and timely identification of malaria patients, their hospitalization and treatment are also measures to prevent the epidemic.
Instructor-valeologist Natalya Dudarchik
Classification
As noted above, there are separate types of parasitic pathogens of the disease. Each form of infection can provoke the development of pathologies with its own specific characteristics. To avoid confusion when diagnosing and drawing up a treatment program, the following classification of malarial plasmodium has been developed:
- Malariae-malaria is an infectious pathogen characterized by an incubation period of 4 days.
- Plasmodium vivax is a three-day variant of malaria.
- Plasmodium ovale is another form of the pathogen, when infected, the first symptoms appear within 3 days.
- Falciparum is a tropical type of infection.
- Plasmodium knowlesi is the most dangerous class of malaria pathogen, since in this case the phase of active reproduction of the parasite in the host’s blood begins after 24 hours.
Intermediate host
You may be interested in: “Dermazol” (ointment): instructions for use, reviews
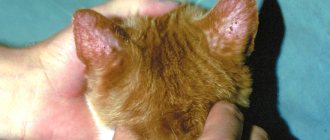
The main host of Plasmodium falciparum, which is the mosquito, transmits the causative agents of the disease to humans during a bite. Microscopic parasites quickly spread through the bloodstream throughout the body, concentrating in the liver tissues. Here the stage of asexual reproduction is activated. The result is the formation of so-called merozoites, which infect red blood cells, actively absorb hemoglobin and multiply intensively.
Subsequently, the parasite leaves the red blood cells. It forms digestive vacuoles where nutrients are concentrated. During the processing of food by a pathogenic microorganism, toxins are formed that enter the blood along with the products of its vital activity.
The above stages are repeated periodically. During such cyclical processes, unpleasant symptoms of the disease appear, from which the intermediate host begins to suffer. The malarial plasmodium eventually reaches the apogee of its development, transforming into gametocytes. With the next mosquito bite, the parasites in the presented form penetrate back into the insect’s body, where they return to active sexual reproduction.
Main owner
To form a sporogonium capable of reproduction, the malarial plasmodium must enter the body of a female Anopheles mosquito, which lives in the tropical regions of the planet. It is these insects that act as the main host of malarial plasmodium.
Inside the mosquito's body, the microscopic parasite divides, during which independent female and male cells are formed. Each of them has one set of chromosomes. When gametes of individual sexes fuse, cells with a complete chromosome complement are formed. The latter are presented in the form of elongated zygotes. They are extremely mobile, which allows them to penetrate into the tissues of the mosquito’s body, where new incubator cells are formed, covered with a protective membrane. Hundreds of sporangia develop in such containers. After maturation, the walls of the incubator are torn. Single-celled parasites begin to move to the salivary glands of their main host. The malarial plasmodium subsequently seeks to enter the human body.
Methods for eliminating infection
The most effective pharmacological agent, the active substances of which slow down the vital processes of malarial plasmodium in the human body, is the drug quinine. The parasitic infection is also low resistant to the substance artemisinin, which is synthesized from the wormwood plant.
To relieve the main symptoms of the disease, the drug primaquine is often prescribed. It is also used for the final destruction of sporangia of the infectious agent in the body.
As you can see, there are several pharmacological drugs to combat Plasmodium falciparum. Despite the availability of drugs on the market, epidemics of the disease are still quite common in tropical regions of the planet. The reason is often the reluctance of the population of underdeveloped countries to use drug treatment, despite the fact that the costs of purchasing effective drugs are often insignificant.
Finding out the cause of the disease
In 1880, French military doctor Charles Louis Alphonse Laveran, working in Algeria, suggested that malaria was caused by protozoa. This was the first time that protozoa were identified as the cause of disease. For this and other discoveries he was awarded the Nobel Prize in Physiology or Medicine in 1907. The genus name of the parasite Plasmodium was proposed in 1895 by Italian scientists Ettore Marchiafava and Angelo Celli. A year later, Cuban doctor Carlos Finlay, who was treating yellow fever patients in Havana, first suggested that the disease could be transmitted to humans by mosquitoes. The Englishman Sir Ronald Ross, working in India, showed in 1898 that certain species of mosquitoes transmit malaria to birds, and isolated parasites from the salivary glands of the mosquito. He also managed to find parasites in the intestines of mosquitoes that fed on the blood of sick people, but was unable to trace the transmission of parasites from mosquitoes to humans. In 1898, Giovanni Batista Grassi managed to experimentally infect a person with malaria through a mosquito bite (he experimented on volunteers, including himself). He also proved that only mosquitoes of the genus Anopheles are carriers of malaria in Italy, and developed and implemented measures for the prevention of malaria. However, in 1902, only Ronald Ross received the Nobel Prize in Medicine for describing the life cycle of the malaria parasite. The data obtained by Finlay and Ross were confirmed in 1900 by the medical council, headed by Walter Reed. The recommendations of this council were used by William C. Gordas for the health measures carried out during the construction of the Panama Canal.
Mosquito nets and repellents
Mosquito net is an effective measure against malaria
Mosquito nets help keep mosquitoes away from people and thereby significantly reduce the number of infections and transmission of malaria. Nets are not a perfect barrier, so they are often used in conjunction with an insecticide that is sprayed to kill mosquitoes before they find their way through the net. Therefore, insecticide-impregnated nets are much more effective.
Covered clothing and repellents are also effective for personal protection. Repellents fall into two categories: natural and synthetic. Common natural repellents are essential oils of certain plants.
Examples of synthetic repellents:
DEET (active ingredient - diethyltoluamide) (eng. DEET, N,N-diethyl-m-toluamine)
Destruction of mosquitoes
Efforts to control malaria by killing mosquitoes have achieved success in some areas. Malaria was once common in the United States and Southern Europe, but the draining of swamps and improved sanitation, along with the control and treatment of infected people, have removed these areas from being unsafe. For example, in 2002, there were 1,059 cases of malaria in the United States, including 8 deaths. On the other hand, malaria has not been eradicated in many parts of the world, especially in developing countries - the problem is most widespread in Africa.
DDT has proven itself to be an effective chemical against mosquitoes. It was developed during World War II as the first modern insecticide. It was first used to fight malaria and then spread to agriculture. Over time, pest control, rather than mosquito eradication, has come to dominate the use of DDT, especially in developing countries. Throughout the 1960s, evidence of the negative effects of its misuse increased, eventually leading to the ban of DDT in many countries in the 1970s. Prior to this time, its widespread use had already led to the emergence of DDT-resistant mosquito populations in many areas. But now there is the prospect of a possible return of DDT. The World Health Organization (WHO) now recommends the use of DDT against malaria in endemic areas. In addition, the use of alternative insecticides in areas where mosquitoes are resistant to DDT is proposed to control the evolution of resistance.
Story
It is believed that people have been suffering from malaria for 50,000 years. Malaria is believed to be native to West Africa (P. falciparum) and Central Africa (P. vivax). Molecular genetic evidence suggests that the preparasitic ancestor of Plasmodium was a free-living protozoan capable of photosynthesis that adapted to live in the intestines of aquatic invertebrates. It could also live in the larvae of the first blood-sucking insects of the order Diptera, which appeared 150-200 million years ago, quickly acquiring the ability to have two hosts. With the advent of humans, malaria parasites evolved that were capable of changing hosts between humans and mosquitoes of the genus Anopheles. The oldest mosquito fossils found containing remains of malaria parasites are 30 million years old.
The first chronicled evidence of fever caused by malaria was discovered in China. They date back to approximately 2700 BC. e., during the reign of the Xia dynasty.
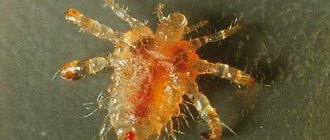
The structure of the parasite
You may be interested in:Main types of hernias
The development cycle of such a parasite is reflected in the structure of the malarial plasmodium. In the early stages, the infectious agent is presented in the form of so-called schizonts. This asexual form of the parasite has the appearance of a ring, which consists of a nucleus and rough cytoplasm surrounded by a vacuole. Subsequently, the microorganism develops pseudopods. A sexually mature malarial plasmodium lacks a vacuole, and the cytoplasm acquires a reddish tint due to the absorption of hemoglobin from the host’s blood.